Finding better answers means asking better questions. Nowhere is this truer and more consequential than with questions surrounding matters of life and death. By asking better questions about care for the terminally ill, Dame Cicely Saunders (1918–2005)—a British nurse, social worker, and physician—founded the modern hospice movement.
In a time when medically assisted suicide is on the rise, and the conditions that qualify for its application broaden, we should remember the vocation and accomplishment of the doctor who gave birth to the modern hospice movement.
It was, in fact, a question asked by a dying patient under Saunders’ care early in her career that led her to some of these better answers. In 1948, a 40-year-old patient with an incurable cancer named David Tasma asked Saunders during a bout of sadness as he faced impending death, “Can’t you say something to comfort me?”
Comfort: That was the question. It was also the answer.
Through her experience with this patient—along with the years of education, research, and practice that followed—Saunders came to understand that those who are dying need comfort, not only to alleviate their physical suffering, but also to meet their unique emotional, spiritual, and social needs. The terminally ill need total care for what Saunders called “total pain.”
Such an understanding is axiomatic today. Yet this was not the case when, merely decades ago, Saunders challenged and changed the medical profession’s approach to end-of-life care. To appreciate the significance of Saunders’ legacy, it helps to understand the state of medicine in her lifetime, particularly as it was practiced when confronted with the terminally ill.

A Cure the Only “Success”
The rise of modern medicine occurred alongside the growth of the Industrial Revolution, which began in the late 18th century. Modern medicine was marked by rapid advances in medical technology and pharmaceutics, along with increasingly effective prevention and treatment of infectious diseases and other illnesses. But like modernity itself, modern medicine was founded on an underlying presumption of continual progress. Indeed, advances in medicine have proceeded at a dizzying pace over the past two centuries. But medicine cannot, in the end, eradicate death. And within a paradigm in which “success” has almost always meant “cure,” an illness or condition that can’t be fixed signifies failure. Research, energy, and resources devoted to cases that represent “failure” have simply not been a priority for most of the history of modern medicine. In order for “success” to include those for whom treatment would not bring a cure, the definition of success had to change. Saunders helped make that change.
She did so, not coincidentally, during the years in which public debates around euthanasia were on the rise. Euthanasia, suicide, and medically assisted death have taken place since ancient days, of course. But late modernity saw new and seemingly more sophisticated approaches to these age-old questions.
The origin of the modern-day euthanasia debate is usually marked with a speech given in 1870 at the Birmingham Speculative Club in England by a man named Samuel Williams, a schoolteacher, not a doctor, but who sparked vigorous debate within the medical profession. The year 1935 brought the founding of the Voluntary Euthanasia Legalisation Society in Britain. Just a few years later, in 1939, an infant born with severe disabilities was killed in Germany in what was later characterized as the first state-sponsored act of euthanasia, the first of many such acts under the Nazi regime. It wasn’t long before the United States entered the debate with a proposal to legalize euthanasia in New York in 1947. It proved unsuccessful but garnered enough support for the cause to gain momentum.

It was in such a climate that Cicely Saunders entered the world stage, transforming the medical profession’s understanding of what it means to treat patients successfully who will not live. To look back on Saunders’ life is to see that, perhaps, such an accomplishment could be done only by someone like her, a woman not working within the academy or in the laboratory, but in the trenches of end-of-life care, a woman who brought her whole life and personality to her work and to her patients.
An Outsider’s Perspective
Those who knew her describe Saunders as relentless, passionate, intense, and intimidating. Standing nearly six feet tall, she carried the fierceness of her personality bodily as well as inwardly. Yet she was also known to be naturally and deeply intuitive and empathetic. This empathy is attributed to her own experiences early in life feeling like an outsider, lonely and unpopular. Sent to boarding school, she would later describe herself in an interview with the BBC as being unhappy while away at school and just as unhappy at home.

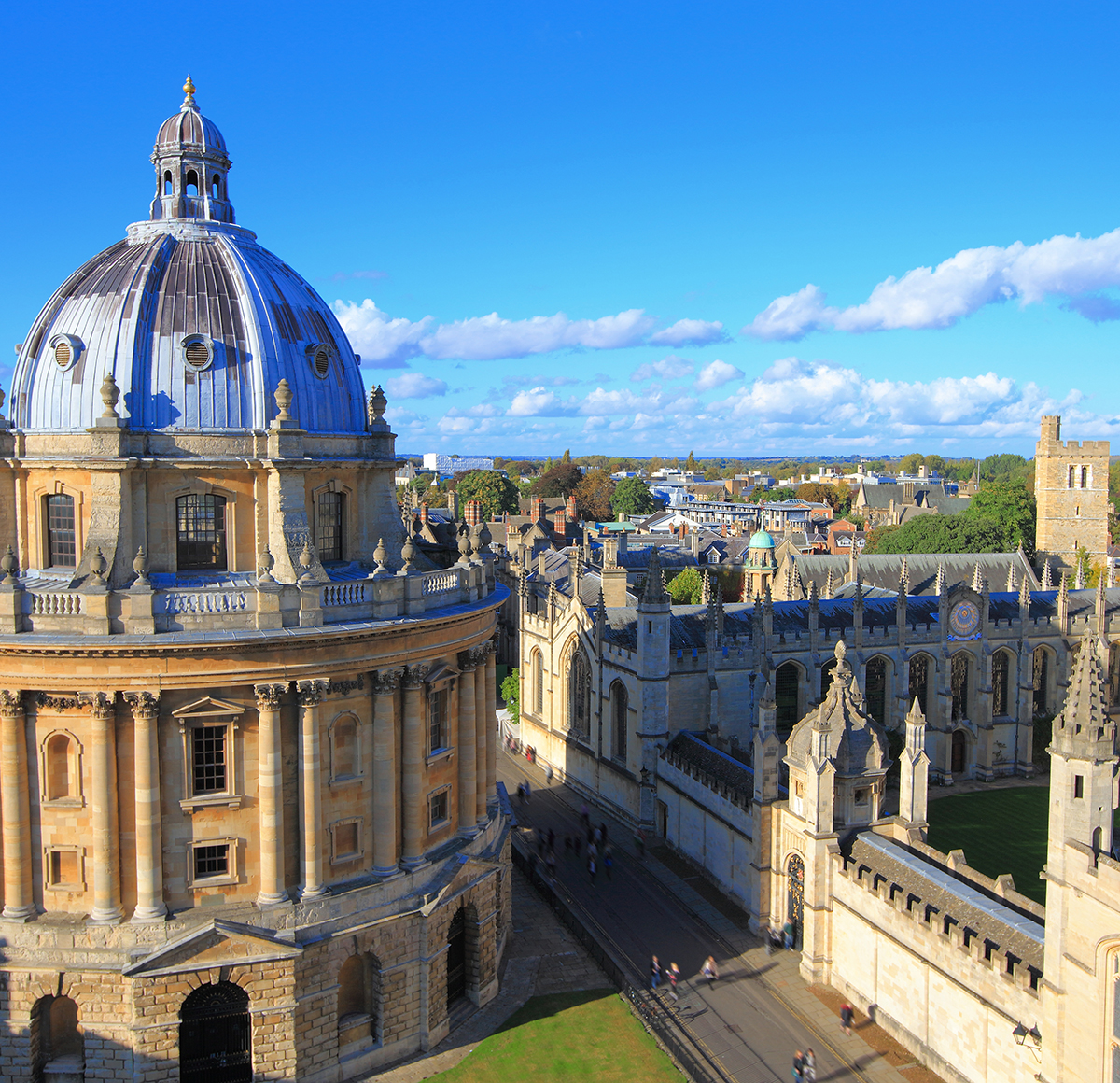
Saunders stubbornly refused to follow the path of least resistance, a quality made obvious early on when she left Oxford University after her first year of study to enter the nursing profession. At Oxford, she had been enrolled in a politics, philosophy, and economics program. But then the Second World War broke out, and Saunders wanted to help the effort in a practical way. To enter nursing, however, would directly defy the wishes of her parents, an unhappily married but well-to-do and upwardly mobile couple who wanted greater accomplishments from their firstborn than mere laboring like a commoner, which is how they viewed nursing. Saunders would also be disappointing her school. One biographer records that an administrator at Oxford, upon learning of Saunders’ plan to drop out and her reason for doing so, declared it was “a great pity” for Saunders to abandon her university studies “to take up work which, although extremely useful, can at the present be adequately fulfilled by a large number of people.”
Saunders would not be deterred. Instead, she would make history.

Upon leaving Oxford, Saunders undertook her nursing training at St. Thomas’ Hospital in London in the historic program established by Florence Nightingale in 1860. She worked as a “Nightingale nurse,” as they were called, until 1944, when the spinal problems that had plagued her most of her life resulted in a back injury that made nursing, with its rigorous physical demands, an impossible pursuit. What seemed at first to be a terrible misfortune, however, led to a path Saunders would never have anticipated or planned.
She returned to Oxford and took a degree as an almoner (or social worker), allowing her to continue caring for people in a hospital setting without the toll nursing would take on her body. It was during her work as an almoner that Saunders met Tasma, the man who opened her eyes to the needs of the dying—and opened her heart, for the first time, to romantic love, albeit briefly and chastely. As a Jewish Pole—a refugee from the Warsaw Ghetto—Tasma was an outsider, too. The personal connection the two shared seemed both unexpected and inevitable. Tragically, Tasma died just six weeks after the two met. But in that abbreviated time, Saunders and Tasma not only came to love one another but also staked out a vision for better meeting the needs of the terminally ill. Upon his death, Tasma bequeathed to Saunders 500 pounds, seed money that would bear fruit years down the road.
‘It’s the doctors who desert the dying.’
But first Saunders had more work and more learning to do. She volunteered at St. Luke’s Home for the Dying, where she observed techniques for pain control that were novel then but are standard today. These practices included giving analgesics at regular intervals rather than making the patient wait until the pain was too much to endure. They included giving medicine orally rather than through injection as much as possible to offer greater ease for both patient and caregiver. And it was while working at St. Luke’s that Saunders received advice that made the fullness of her legacy possible. Saunders’ brother Christopher noted in a biographical essay that she had been trying to figure out what path to take in medicine when a highly regarded surgeon told her, “Well, you’ve got good ideas, but you won’t get anywhere unless you become a doctor. It’s the doctors who desert the dying.”
If Saunders was going to change the way doctors treated the dying, she would have to become one.
Once more she returned to school. By then she was 33. With classmates far younger than she, Saunders was an outsider again. She was also among a tiny percentage of female medical students. She finished her training and qualified as a doctor at age 38.

In 1958, as a newly minted physician, Saunders quickly staked out her ground in end-of-life care. As the British Medical Journal reports, Saunders published an article complaining, “It appears that many patients feel deserted by their doctors at the end.” She proposed instead that medical teams “work together to relieve where they cannot heal, to keep the patient’s own struggle within his compass and to bring hope and consolation to the end.” Right out of the gate, Saunders made her mark, striking against the status quo within the medical establishment.
A Shelter for the Dying
Saunders is considered the founder of the modern hospice movement because hospice itself was not new. She pioneered in bringing modern understandings of not only medicine but also psychology, education, and research to bear on care for the dying. But places for the dying, the original sense of “hospice,” had long existed. The word hospice comes from a Latin root that means “host” (with etymological connections to “stranger,” “guest,” “visitor,” and “sojourner”). It is believed that the earliest hospices were places where those making the arduous pilgrimage to the Holy Land could stay to receive shelter and care if they fell ill (often fatally) along the way. The Middle Ages saw the rise and decline of these rudimentary institutions formally devoted to care for those who were dying, a movement that paralleled the growth and decrease in the number of the religious orders that first established them. With the development of modern medicine in the 19th century, a number of modern hospices were opened in the United Kingdom (and elsewhere) to house those dying of tuberculosis or other incurable diseases.
‘Hospice isn’t just a building. Hospice is a philosophy of care.’
As the history of the word reflects, the concept of hospice care since its inception had always signified a shelter for the dying. Shelter in this sense was literal: it was a place—with a bed, a roof, food, and water—where a dying person could take last breaths, a place to relieve that physical body from as much suffering as possible. The shift that Saunders brought to hospice moved this narrower concept from that of merely a place to a broader mode of care. Today hospice refers to the holistic end-of-life care Saunders advocated, whether administered in a hospital, care facility, or at home.“Not everybody has buildings,” Saunders explained upon being awarded the Conrad N. Hilton Humanitarian Prize in 2001. “Hospice isn’t just a building. Hospice is attitudes and skills. Hospice is a philosophy of care.”
Thus, Saunders opened St. Christopher’s Hospice in southwest London in 1967, following years of research, planning, and financing. She insisted on building the hospital from the ground up because she didn’t want simply to house and care for the terminally ill, though such places were certainly worthy and needed. But these already existed. St. Christopher’s was the world’s first hospital devoted not only to serving the terminally ill but also to teaching and research in end-of-life care. More than a place, hospice would become, according to Saunders’ visionary plan, a way to live while facing death. The architecture of St. Christopher’s made real Saunders’ vision for what the end of life could and should be like. The facility featured spaciousness, light, gardens, and room to accommodate patients’ family members, so they, too, could be cared for while being with their loved ones. It was the first facility in the world built to accommodate teaching and research in the field of end-of-life care.

St. Christopher’s also helped birth the field of medicine now called palliative care. Balfour Mount, a Canadian physician who coined the phrase in 1974, visited the hospital to research Saunders’ work and to apply it to the work he had already been undertaking in the area of pain management, which includes but is not limited to cases of terminal illness. Thus, in founding the modern hospice movement, Saunders helped bring about a field of medicine that would offer even more comfort to those facing death.
Flipping the Christian Switch
Just as the first hospices were religious in nature, so, too, Saunders’ religious faith played a key role in her life’s work. Saunders’ childhood home and upbringing were not at all religious. Nor did Saunders seem to be seeking any kind of religious experience at first. In fact, du Boulay notes in her biography that, after reading George Bernard Shaw in grade school, Saunders declared herself an atheist. But in 1945, after she’d returned to Oxford to become an almoner, Saunders befriended Christian classmates who also happened to be evangelicals. It was also around this time that Saunders’ parents were going through a painful separation. When she accompanied these evangelical classmates on a holiday, Saunders found herself reluctantly taking them—and their faith—seriously. As she later described it, “The switch was flipped.” Saunders went all in. According to du Boulay, she read C.S. Lewis and Dorothy Sayers, met Charles Williams, and joined the Socratic Society at Oxford, C.S. Lewis’ gathering of atheists and Christians. Eventually, she became a member of John Stott’s church, All Souls, in central London. Saunders would also broaden her Christian views—particularly by the time, late in life, she met and eventually married a Polish artist and professor who was Roman Catholic.
But even as far back as her friendship with David Tasma, whose background, as already noted, was Jewish, Saunders never sought to proselytize her patients, whether those under her direct care or those within the care of her hospital or within the movement she launched. When Tasma asked her for comfort, she looked to his Jewish background and recited Psalms to him, and Tasma later reported that he felt at peace with God. Among the needs of the dying, Saunders recognized the realm of spiritual needs and included these in her understanding of total care. But she knew those needs could be met only on the terms of the patient—just as was true of their individualized physical, emotional, and social needs.
This was what Saunders meant by the concept of “total pain,” an approach to suffering that takes into consideration its physical, psychological, social, and spiritual elements. Saunders developed this understanding under the influence of Elisabeth Kübler-Ross’s research on the stages of grief. And grief, Saunders recognized, is a significant source of the pain that accompanies dying. Understanding the role of grief in dying, and all its sources, helped Saunders speak clearly and prophetically against the growing push toward physician-assisted death taking place in her lifetime. In one television interview, she argued that legalized euthanasia
… would pull the rug out from under a great many vulnerable people who would so easily feel, “Well, I have a right to shorten my life. Now, I have a duty to do it because I am a burden on others and because my life as part of society is now worthless.” And I feel very strongly that we need to say to people, “You matter because you are you. And you matter to the last moment of your life. And we will do all we can to make that life as good as we can.”
MAID in Canada
Saunders’ recognition of “total pain” is essential for today’s discussion of end-of-life care, especially when those discussions turn to the willful ending of life as part of medical practice, as they are increasingly today.
Canada is a current focal point of these discussions. Now offering assistance to both terminally ill and chronically ill patients, Canada has some of the most liberal assisted death laws in the world. As reported by multiple news outlets last year, medically assisted deaths accounted for 4% of all deaths in Canada in 2022. The total number of these deaths beginning in 2016, when physician assisted death was legalized there, through 2022 is 44,958.
Saunders recognized the realm of spiritual needs and included these in her understanding of total care.
What is happening in that nation sheds light on what is happening or is likely to happen in many places throughout the world. While laws and terminology vary, active euthanasia in some form is currently legal in five countries: Belgium, the Netherlands, Luxembourg, Canada, and Colombia. Passive euthanasia is legal in these five countries as well as the following: Switzerland, Germany, Austria, Norway, Sweden, Spain, Mexico, Argentina, and Chile. Physician-assisted suicide is legal in seven countries: Belgium, the Netherlands, Luxembourg, Switzerland, Germany, Finland, Canada, and Japan. In the United States, medically assisted suicide is legal in 10 states and the District of Columbia.
Although terms differ across the globe and are ever-shifting as laws change, Canada’s government-sanctioned program for medically assisted death is called MAID—Medical Assistance in Dying. The Canadian government defines it this way: “Medical assistance in dying (MAID) is a process that allows someone who is found eligible to be able to receive assistance from a medical practitioner in ending their life.” Among other requirements, to qualify for MAID, a person must “have a grievous and irremediable medical condition, make a voluntary request for medical assistance in dying,” and “give informed consent to receive medical assistance in dying.” Canada offers two forms of assistance in dying:
Method 1: a physician or nurse practitioner directly administers a substance that causes death, such as an injection of a drug. This is sometimes called clinician-administered medical assistance in dying.
Method 2: a physician or nurse practitioner provides or prescribes a drug that the eligible person takes themselves, in order to bring about their own death. This is sometimes called self-administered medical assistance in dying.
What the Canadian government calls “Method 1” is, in fact, euthanasia. “Method 2” is medically-assisted suicide. The term “medical assistance in dying” draws attention away from these other words that carry moral weight and social stigma. The moral actions themselves haven’t changed, even if the techniques, vocabularies, and popular acceptance of them have.
MAID became legal in Canada in 2016 under certain conditions. Those conditions were broadened in 2021 and will be further loosened this year to allow those who suffer only from mental illness (unaccompanied by other illness) to seek medically assisted death.
In a story covering this development last year, the New York Times interviewed Dr. John Maher, a psychiatrist in Barrie, Ontario. Maher specializes in treating complex cases of mental illness, the kinds of cases that can be improved but often only over the course of years and intense treatment. It is easy for such patients to lose hope. Maher told the Times that he is concerned that these kinds of patients will look to assisted death rather than pursuing extended treatment. “I’m trying to keep my patients alive,” he was reported as saying. “What does it mean for the role of the physician, as healer, as bringer of hope, to be offering death? And what does it mean in practice?”

Hopelessness has many causes, some more possible to fix than others. In 2022 a Canadian man named Amir Farsoud sought medical assistance in dying because of his poverty and impending homelessness. Because Farsoud suffers chronic back pain, he is eligible for MAID, but it was not the physical pain from his chronic condition that was the source of his most intense suffering. Rather, Farsoud’s overwhelming pain came from the failure of any social support system to meet his basic living needs. He faced losing his home. This led him to feel death was the only way out. But when the story of his plight made headlines, Farsoud received such an outpouring of public support, including more than $60,000, that his outlook on life (and death) changed. But it wasn’t just the money. “There has been this amazing outpouring of love and support, emotional support,” he told City News.
Cicely Saunders knew the intensity of the kind of pain that Farsoud suffered. And she knew how such pain could be comforted and how that comfort could revive the desire to live. By showing how the pain that comes from dying can be identified and alleviated, Saunders’ work bears significant application to individuals who choose to hasten their deaths because their pain is unbearable.
Wherever medical science is oriented entirely toward cures, those who suffer from incurable conditions will become extraneous or even expendable. Wherever medical care focuses solely on physical suffering, other forms of human suffering will be inadequately addressed. Of course, human suffering can never be entirely eradicated. But wherever scientific knowledge sees no purpose in suffering, then those who suffer can be understood as having no purpose as well.
Medical science, care, and knowledge are all rooted in human actions and understanding. Humans do not have total power over death or dying. But humans have power over how we care for one another, whether or how we comfort pain, whatever its source, and over the meaning and purpose we assign to our living and to our dying.
It has not been even 20 years since Cicely Saunders’ death. (Poignantly, fittingly, it was at St. Christopher’s that Saunders herself spent her own last days, dying of breast cancer on July 14, 2005.) But her life and work deserve to be remembered and retold not only for the changes she effected in the past but also because her wisdom, her practical solutions, and her sheer faith in human potential—even at the natural end of life—can still inform discussions today.
For Further Reading
Buchholz, Katharina. “Where Most People Die By Assisted Suicide.” Forbes, Aug. 12, 2022.
Clark, David. Cicely Saunders: A Life and Legacy. Oxford University Press, 2018.
“Dame Cicely Saunders,” Thames Television. Video. 1983.
Du Boulay, Shirley. Cicely Saunders: The Founder of the Modern Hospice Movement. Hodder and Stoughton, 1984.
Du Boulay, Shirley. Changing the Face of Death. Religious Education Press, 2001.
Isai, Vjosa. “Death by Doctor May Soon Be Available for the Mentally Ill,” The New York Times, Dec. 27, 2023.
“Maureen Lipman on Dame Cicely Saunders.” BBC Great Lives. Podcast. Sept. 7, 2016.
“Ontario Man Not Considering Medically-Assisted Death Anymore After Outpouring of Support.” City News, Nov. 17, 2022.
Richmond, Caroline. “Dame Cicely Saunders, Founder of the Modern Hospice Movement, Dies.” The British Medical Journal, July 18, 2005.
Saunders, Christopher. “Dame Cicely Saunders: A Brother’s Story.” Cicely Saunders International. https://cicelysaundersinternational.org/dame-cicely-saunders-a-brothers-story/.




